Insight Blog
Agility’s perspectives on transforming the employee's experience throughout remote transformation using connected enterprise tools.
29 minutes reading time
(5701 words)
Top Communication Challenges in Healthcare – United Kingdom: Fix These 7 Issues Before They Turn Into Major Compliance Failures
Top Communication Challenges in Healthcare – United Kingdom: Fix These 7 Issues Before They Turn Into Major Compliance Failures
Discover the top communication challenges in healthcare in the United Kingdom and how to fix them before they create compliance risks, delays, and patient-care failures.
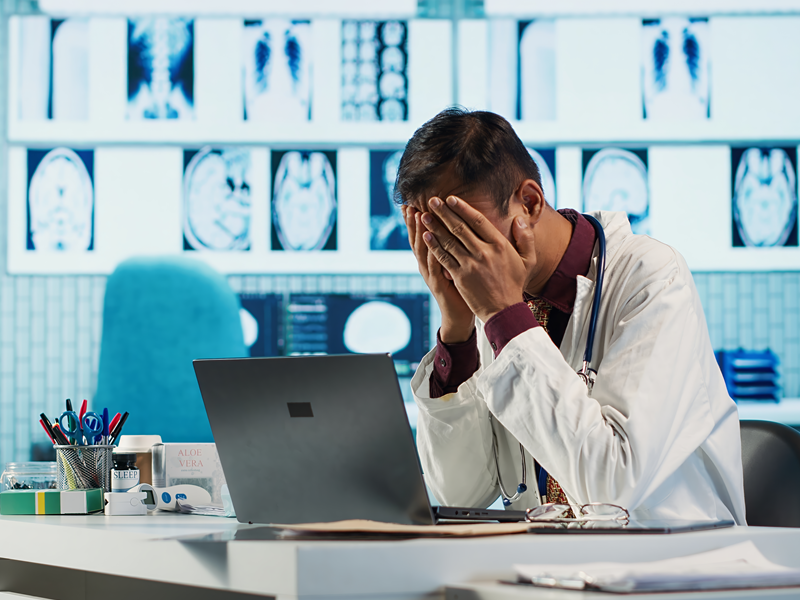
If you work in healthcare in the United Kingdom, you already know the pressure is nonstop.
Staff shortages, rising patient numbers, and tighter compliance rules — it all piles up, and the cracks always show in the same place: communication.
And let's be real… poor communication in healthcare isn't just frustrating. It's dangerous.
According to NHS data, around 70% of serious incidents are linked to communication failures.
Add the millions lost each year to avoidable delays, duplicated work, and constant misunderstandings, and it's clear why healthcare communication united kingdom is such a critical issue right now.
Most healthcare teams aren't failing because they lack skill.
hey're failing because they're forced to communicate using outdated tools, siloed departments, and processes that fall apart the moment things get busy.
That's why in this article, we're breaking down the Top Communication Challenges in Healthcare – United Kingdom, the real reasons these problems keep happening, and — more importantly — how to fix each one before it turns into a major compliance issue.
By the end, you'll know exactly what's slowing down your teams and the practical steps you can take to turn it around fast.
What is communication in healthcare
If you're wondering "What is communication in healthcare?", the answer is simple — but the impact is huge.
Communication in healthcare refers to how information is shared between clinicians, staff, patients, and departments to ensure safe, effective, and coordinated care.
But in practice, it's much more than talking or sending messages.
In the UK healthcare system — whether NHS or private — communication is the backbone of:
- patient safety
- clinical decision-making
- care continuity
- teamwork
- compliance
- staff wellbeing
Without strong communication, even the most skilled clinical teams struggle.
With it, everything becomes smoother, safer, and more consistent.
In healthcare, communication isn't optional — it's a clinical skill.
When communication breaks, patient care breaks.
Strong communication enables:
- accurate handovers
- faster emergency escalation
- fewer medication errors
- safe discharge planning
- clear roles between departments
- collaboration across multidisciplinary teams
- better patient understanding of their treatment
- improved staff confidence and reduced burnout
According to NHS England, poor communication is a contributing factor in 70% of serious incidents, making it one of the most critical safety challenges in the UK.
Read this article: : Top 6 AI-Powered Project Management Tools To Use In 2023
#1. Siloed Communication Between Clinical, Admin, and Support Teams
If you've worked in a UK healthcare setting for even a short time, you've seen how fragmented communication can be.
Clinical, administrative, and support teams all operate with different systems, different workflows, and different communication habits.
What should be a smooth, coordinated flow of information ends up becoming a maze — and that fuels mistakes, delays, and compliance issues across the board.
Siloed workflows are one of the biggest weaknesses in healthcare communication in the united kingdom, and they're at the root of many safety and performance problems.
The Problem
In most hospitals and care settings, departments operate in isolation:
- Clinical teams use one system
- Admin teams rely on email, shared drives, and spreadsheets
- Support teams often depend on paper, WhatsApp, or manual requests
Because these systems don't talk to each other, people don't talk to each other.
This leads to:
- missed updates
- duplicate work
- inconsistent information
- delays during shift changes
- messages being routed to the wrong people
- critical patient details stuck in one department instead of shared
It's not a people problem — it's a structural problem.
The Real-World Impact (Data & Statistics)
Enter yoSiloed communication causes serious, measurable damage in UK healthcare.
According to NHS Improvement and the National Patient Safety Agency:
- 70% of serious incidents include communication failures
- 29% of treatment delays are caused by internal miscommunication
- Staff lose 30–60 minutes per shift searching for missing information
- Communication breakdowns cost the NHS over £1.5 billion per year in avoidable inefficiencies
That's time, money, and — most importantly — patient safety on the line.ur text here ...
Why Healthcare Teams in the UK Become Siloed
Silos aren't created intentionally — they grow out of everyday pressures.
Some of the biggest contributors include:
- Teams working under intense pressure with little time to coordinate
- Legacy systems that don't integrate
- Heavy reliance on paper or outdated tools
- Staff turnover and temporary agency staff
- Different departments having different communication cultures
- Shift-based work where information is verbally passed down
The result?
Teams only see their part of the picture, not the whole.
The Risks for Healthcare Communication United Kingdom
When communication breaks down, the risks spread quickly:
- Compliance failures due to outdated or missing information
- Patient safety incidents caused by incomplete or incorrect updates
- Longer waiting times, especially between clinical and admin tasks
- Inconsistent care pathways across wards
- Reduced coordination between labs, imaging, pharmacy, and clinical teams
- Increased stress + burnout for staff who constantly chase information
These risks compound over time and create a culture where preventable mistakes become normal.
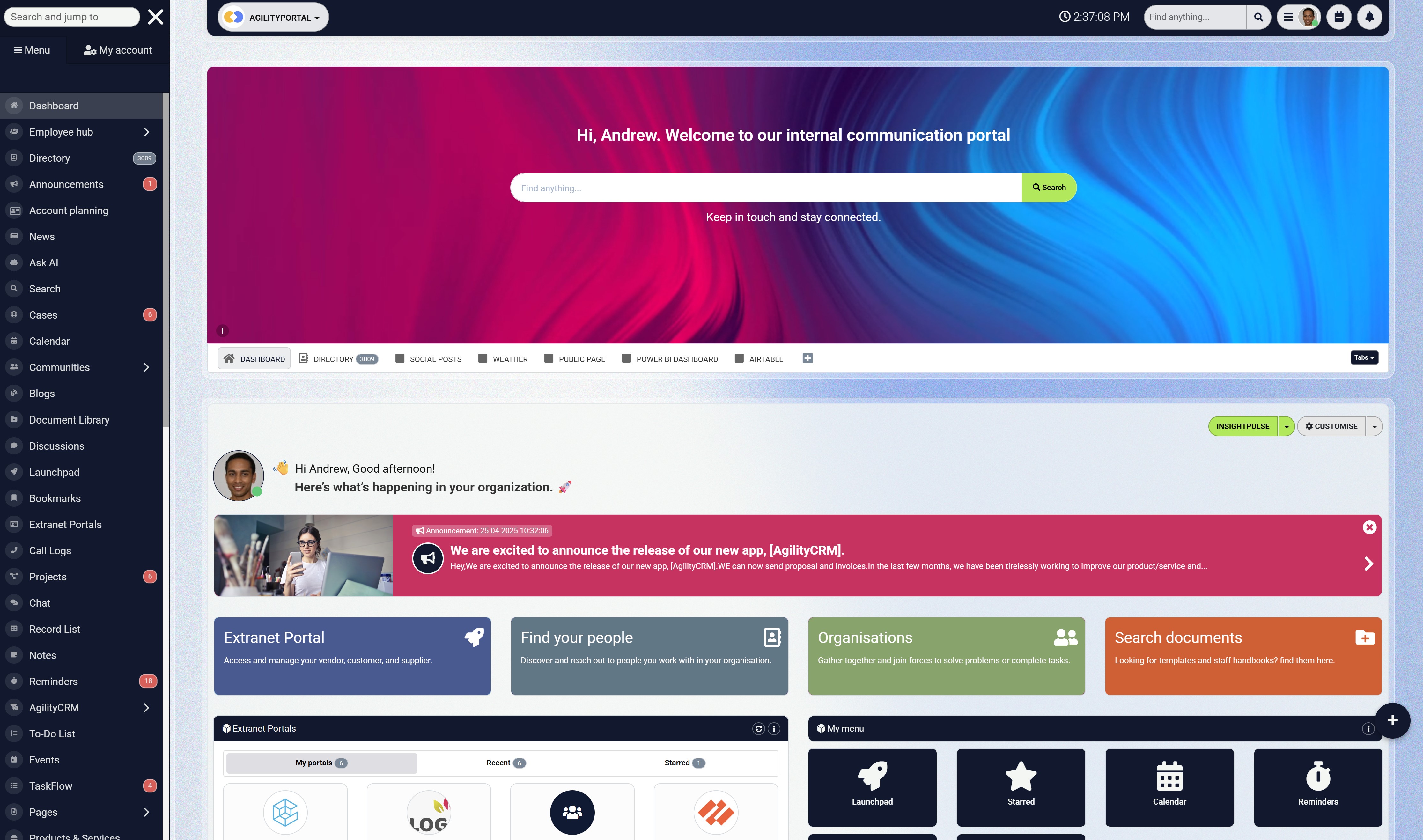
The Solution: A Centralised Digital Hub With AI-Powered Search
The only real way to eliminate silos is to bring everyone — every team, every department, every role — into one unified communication platform.
A centralised digital hub ensures:
- everyone sees the same updates
- everyone accesses the same documents
- everyone receives the same communication
- everyone works from one version of the truth
This is how healthcare communication united_kingdom becomes predictable, consistent, and safe.
AgilityPortal provides exactly this: a unified, AI-powered digital workspace built to connect clinical, admin, and support teams in real time, without relying on outdated tools.
Real-Time Communication in One Place
- No more email chains.
- No more lost messages.
- No more siloed conversations.
Every team — wards, clinical staff, admin, estates, pharmacy, labs — communicates in one shared space with channels, notifications, and instant updates.
AI Search That Instantly Finds Any Document or Update
Staff shouldn't waste time searching folders, inboxes, or shared drives.
AI-powered search lets teams instantly find:
- policies
- clinical guidelines
- care pathways
- forms
- announcements
- shift updates
If it exists, they can find it in seconds — even while on the move.
Role-Based Permissions for Patient-Safe Sharing
Not every team needs access to everything.
Role-based permissions ensure:
- clinical staff see clinical updates
- admin sees operational tasks
- support teams see relevant info only
This keeps communication clean, safe, and fully compliant.
Full Audit Trails for Compliance Readiness
For compliance teams, this is huge.
Every update, every message, every document is:
- time-stamped
- version-controlled
- traceable
If regulators ask, "Who saw this update and when?" — the proof is already there.
Expected Improvements After Implementation
When organisations adopt a centralised communication hub:
- Duplication drops by up to 40%
- Shift handover errors fall significantly
- Information hunting time drops by 30–60 minutes per staff member per shift
- Compliance adherence increases due to correct, visible documentation
- Patient flow improves because teams are aligned
- Staff stress and burnout decline thanks to clearer communication
In short:
Better communication = safer patients, happier staff, and fewer compliance risks.
#2. Outdated Tools That Slow Down Critical Care
One of the biggest challenges in healthcare communication united kingdom is the heavy reliance on outdated, disconnected tools — pagers, paper notes, printed handover sheets, email chains, and systems that haven't been upgraded in over a decade.
Even today, over 130 NHS Trusts still use pagers, and many frontline teams rely on manual processes simply because that's how things have always been done.
But outdated tools don't just slow communication — they slow care. In an environment where minutes matter, outdated tech becomes a silent threat.
The Problem With Legacy Communication Tools
Most UK healthcare teams are juggling far too many channels:
- pagers
- shared drives
- EHR systems
- printed forms
- handwritten notes
- verbal updates
That's 6–8 communication channels per shift — none of which talk to each other.
This leads to:
- delayed updates reaching the wrong person
- missed instructions lost in inboxes
- critical information living on paper instead of being shared
- teams duplicating tasks
- confusion during shift changes
- difficulty coordinating across departments
The more outdated the tools, the more fragmented the care.
The Impact on Speed, Safety, and Patient Outcomes
Data shows how damaging outdated communication tools really are:
- 23% of avoidable care delays are linked to poor internal communication tools (NHS Digital, 2024)
- NHS staff lose 48 minutes per shift chasing information that should be instantly available
- The NHS spends £25 million per year maintaining pager systems
- Manual processes contribute to 1 in 5 medication errors (BMJ, 2023)
When tools are outdated, everything slows down — clinical decisions, patient handovers, emergency escalations, and admin workflows.
In critical care, seconds matter. Outdated tools turn seconds into minutes
Why Outdated Systems Still Exist in UK Healthcare
It's not because people want to use outdated tools.
It's because:
- Budget constraints create slow replacement cycles
- Legacy systems are deeply embedded in clinical workflows
- Staff turnover makes it difficult to retrain teams
- New tools often don't integrate with older EHRs
- Many trusts lack a centralised communication strategy
- Paper processes feel "safer" because they're familiar
This creates a cycle where outdated tools continue year after year.
The Data Behind Tool-Related Delays
According to NHS England:
- 31% of emergency alerts do not reach the right team on first attempt
- Paper-based processes add 3–5 minutes to every patient record update
- Emergency response delays increase mortality risk by 8–12% per minute
When communication is slow, patient care is slow — and outcomes decline.
The Solution: A Unified Digital Workspace
The solution is not "more tools."
It's one centralised system built specifically for modern healthcare communication united_kingdom.
A unified digital workspace replaces:
- pagers
- paper handovers
- random WhatsApp groups
- email blasts
- outdated staff noticeboards
- lost documents
- confusing folder structures
…with one integrated platform where communication happens instantly and securely.
AgilityPortal delivers exactly that.
Instant Alerts and Mobile Notifications
Frontline staff don't have time to check email.
Mobile-first alerts ensure:
- clinical updates
- emergency notifications
- escalation requests
- staffing changes
- policy updates
…reach the right person instantly.
This alone cuts response time dramatically.
Integrated Messaging Across All Departments
Instead of juggling 5–7 tools, teams get:
- secure chats
- department channels
- patient-related updates
- cross-department communication
- shared announcements
Everything in one place, no fragmentation.
Centralised Access to All Care Updates
No more hunting through inboxes or folders.
Every document, every update, every policy lives in one home with:
- instant search
- version control
- clear tagging
- audit trails
- mobile access
This cuts wasted time and reduces errors.
The Real Impact of Modern Communication Tools
Healthcare teams using unified digital communication see:
- 40% faster communication during emergencies
- 50% reduction in time spent searching for information
- Better compliance with updated procedures
- Higher staff satisfaction
- Fewer missed updates and errors
When communication improves, patient care improves.
That's the bottom line.
Read this article: : Top 6 AI-Powered Project Management Tools To Use In 2023
#3. Missing or Inconsistent Handover Processes
If there's one moment in healthcare where communication absolutely cannot fail, it's handover.
Whether it's nurse-to-nurse, doctor-to-doctor, ward-to-ward, or day-to-night shift, handover is where vital information is transferred — or lost.
And in many UK healthcare settings, handover is still largely:
- verbal
- handwritten
- rushed
- inconsistent
- undocumented
- dependent on who's on shift
This is one of the biggest silent threats in healthcare communication united kingdom, because one missing detail can completely change patient outcomes.
The Problem With Manual or Verbal Handovers
Manual handovers create huge risks because they depend on:
- tired staff remembering details
- handwritten notes that someone might misread
- verbal summaries during busy changeovers
- pages of paper that get misplaced
- inconsistent templates from ward to ward
Teams simply don't have a structured, standardised format — and that means everyone does it their own way.
Key gaps include:
- incomplete medical histories
- missed lab results
- uncommunicated deterioration signs
- pending tests not being flagged
- unclear discharge plans
- lost medication instructions
A 12-hour shift drains anyone. Expecting perfect memory under pressure is unrealistic — and dangerous.
The Clinical Risk of Inconsistent Transitions
When handovers are inconsistent, mistakes multiply:
- missed treatments
- delayed interventions
- duplicated tasks
- incorrect medication
- unnecessary escalation calls
- delayed discharges
- unclear care ownership
Critical details fall into the cracks, and those cracks widen every shift.
How Handover Gaps Cause Errors in UK Hospitals
Research from the Royal College of Physicians shows:
- 30% of inpatient safety incidents are directly linked to communication failures during handover
- 66% of junior doctors say handover is one of the most dangerous points in the care process
- 1 in 4 medication errors occur during shift transitions
- Staff lose 20–35 minutes per shift correcting incomplete or unclear handover notes
In high-pressure environments, small mistakes become big problems quickly.
The Solution: Structured Digital Handover Templates
The only way to eliminate handover inconsistencies is to remove guesswork.
Structured digital handover templates standardise the process across the entire organisation so every patient handoff includes:
- medical history
- risk factors
- allergies
- outstanding tests
- escalation plans
- medication updates
- care priorities
- notes for next shift
Instead of relying on memory, staff rely on a proven workflow that reduces risk.
AgilityPortal provides these tools natively, making handover safer, faster, and more consistent.
Automated Prompts to Prevent Missed Information
The system can automatically ask:
- "Have you added escalation notes?"
- "Any pending labs?"
- "Any changes in medication since last shift?"
- "Are there outstanding tasks to assign?"
This eliminates human error.
Role-Specific Handover Views
Nurses, doctors, physiotherapists, and admin staff all require different information.
Role-based views ensure each person sees exactly what they need — no clutter, no confusion.
Digital Logging for Audit and Accountability
With digital handovers:
- everything is logged
- managers can review handover quality
- compliance teams have evidence
- errors can be traced
- training needs can be identified
It creates real accountability instead of relying on memory and paper notes.
The Result: Safer, Faster, More Accurate Shift Transitions
Organisations using digital handover processes see:
- 50% fewer handover-related errors
- Consistent communication between shifts
- Better patient continuity of care
- Shorter transition times
- Clearer workload prioritisation
- Reduced stress for incoming staff
It's one of the quickest wins for improving clinical safety.
#4. Poor Visibility Into Policies, Procedures, and Compliance Updates
One of the biggest (and most overlooked) risks in healthcare communication united_kingdom is the inability for staff to quickly access the correct version of policies, procedures, and compliance documents.
In many hospitals and care environments, staff genuinely don't know where the latest information is stored — or whether the document they're using is even the most recent version.
This creates a dangerous environment where outdated processes get followed simply because they're the easiest ones to find.
The Problem: Staff Can't Find the Latest Version
Here's the reality inside most UK healthcare organisations:
- Policies live in old shared drives
- Procedures are emailed as PDFs and never updated
- Staff rely on printouts pinned to noticeboards
- Some teams update documents… but others don't know
- Version numbers are inconsistent or missing
- Compliance teams change processes, but frontline staff never see the update
- People save old files on personal desktops
This leads to a massive, organisation-wide problem:
Everyone is working with different information.
Compliance Risks in a Fast-Changing Healthcare System
Healthcare regulations evolve constantly.
Whether it's:
- infection control
- safeguarding
- digital records
- medication safety
- emergency planning
- data protection
- patient handling
- clinical governance
…healthcare organisations are legally responsible for ensuring everyone is following the correct process.
But how can staff comply when they can't even find the right version?
This has serious implications:
- Staff unknowingly follow outdated procedures
- Trusts fail CQC inspections
- Audit trails collapse
- Investigations uncover missing documentation
- Legal risk increases
- Patients receive inconsistent care
Non-compliance isn't always intentional — most of the time, it's caused by poor document visibility.
What the Data on Outdated Policy Usage in UK Hospitals Says
According to the Care Quality Commission:
- 42% of compliance breaches are linked to outdated or inaccessible information
- 1 in 3 ward managers say it's difficult to ensure staff have the latest policies
- Staff spend an average of 19 minutes searching for the right document
- 67% of nurses say they're unsure if they're using the correct version of a clinical guideline
And these are not small issues — these findings directly affect patient safety and compliance scores.
The Solution: Version-Controlled Document Libraries
The solution is simple but powerful:
A single, centralised, version-controlled library where all policies, procedures, and compliance documents live — with clear ownership and automated updates.
This eliminates confusion immediately.
AgilityPortal delivers this by giving healthcare organisations a structured, searchable, fully managed document system that removes risk and improves clarity.
Automatic Update Notifications
Whenever a compliance document is updated:
- all relevant staff receive notifications
- outdated versions are removed
- the new version replaces all previous links
- managers can track which staff have viewed the update
No more scatter-fed communication. Everyone stays aligned.
Document Expiry Alerts
Healthcare documents often have expiry dates — but teams rarely track them.
AgilityPortal automatically:
- flags upcoming expirations
- prompts managers to review policies
- ensures outdated documents aren't used
- keeps compliance timelines intact
This is critical during audits.
Searchable Policy Repositorie
Instead of digging through folders or inboxes, staff simply type a keyword.
Instantly, they'll find:
- the current version
- the owner
- the date updated
- related procedures
- any linked forms
- the compliance category
It removes friction and saves huge amounts of time.
Why This Matters for Healthcare Communication Companies
When teams have clear visibility:
- compliance improves
- patient care is safer
- clinical errors decrease
- investigations become transparent
- regulators trust the organisation more
- frontline staff feel more confident in their decisions
The right information at the right time isn't a "nice to have" — it's a safety requirement.
The Bottom Line: Clear Information = Safer Healthcare
A centralised, version-controlled document library eliminates:
- outdated documents
- miscommunication
- confusion
- risky decisions
And replaces them with:
- clarity
- consistency
- compliance
- accountability
When policies are easy to find, easy to verify, and easy to update, everything runs smoother — and patients get better, safer care.
#5. Slow Internal Communication During High-Pressure Moments
In healthcare, speed isn't a luxury — it's a requirement. Whether it's a deteriorating patient, a safeguarding issue, a medication error, or an infection control alert, internal communication must reach the right people instantly.
But in many UK healthcare environments, internal communication still relies on outdated or inconsistent methods:
- phone trees
- pagers
- manual escalations
- emails that no one checks during shifts
- shouting across corridors
- sending runners between wards
This creates dangerous delays at the exact moments when time matters most.
It's a major weakness in healthcare communication united_kingdom, and it has life-or-death consequences.
The Problem With Delayed Escalation
Slow communication during emergencies leads to:
- delayed responses
- missed escalation pathways
- confusion about roles
- no visibility into who received the alert
- no way to verify that the message was delivered
- poor coordination between departments
If someone needs urgent assistance, the message needs to reach the right people — not bounce around between outdated systems.
Here's the hard truth:
The system fails before the staff do.
Even the most skilled nurses and clinicians can't compensate for slow, broken communication.
The Impact on Emergency Response
In high-pressure scenarios, slow internal communication creates a chain reaction:
- A deteriorating patient isn't escalated quickly enough
- A critical test result doesn't reach the clinical team
- A medication error goes unreported until shift change
- Infection control alerts go unseen in inboxes
- A mental-health crisis escalates because staff didn't arrive in time
The delays aren't about negligence — they're about the tools.
UK Data on Critical Communication Failures
According to NHS England and the National Patient Safety Alerts system:
- 22% of preventable critical incidents involve communication delays
- 31% of emergency alerts fail to reach the right team on first attempt
- Average delay in escalating deteriorating patients is 8–12 minutes
- Every minute of delay increases mortality risk by 8–12%
- Hospitals using pagers instead of mobile alerts experience 40% slower response times
Slow communication isn't just inefficient — it's dangerous.
The Solution: Mobile-First Real-Time Alerts
Healthcare urgently needs tools designed for the realities of clinical environments — tools that deliver alerts instantly, to the right people, with confirmed delivery.
AgilityPortal solves this by replacing slow, fragmented methods with mobile-first, real-time communication built specifically for healthcare teams.
Escalation Paths for Urgent Communication
AgilityPortal lets organisations design clear, automated escalation workflows:
- deteriorating patient
- code alerts
- missing patient
- safeguarding issues
- urgent infection control
- critical equipment failure
The system automatically pushes the alert through the correct escalation path.
No guesswork. No manual chains.
Push Notifications to the Right Team Immediately
Instead of relying on:
- pagers
- emails
- desk phones
- verbal relays
Staff receive instant mobile notifications, even if they're moving between wards.
Notifications include:
- urgency level
- location
- instructions
- who else received the alert
This cuts response time dramatically.
Confirmed Read Receipts for Safety
Unlike email or pagers, AgilityPortal provides:
- read receipts
- delivery confirmation
- real-time visibility for managers
- instant escalation if someone doesn't respond
This is crucial for:
- Major Incident response
- infection control
- safeguarding
- time-sensitive clinical tasks
- safety investigations
For the first time, leaders know exactly who has seen a critical message.
The Impact of Real-Time Communication on Safety
When healthcare organisations adopt fast, modern alerting tools:
- response times improve by up to 40%
- clinical teams are mobilised faster
- emergency decisions happen sooner
- escalations become consistent
- patient deterioration is caught earlier
- cross-department coordination becomes smoother
The difference is dramatic.
It's the closest thing to an immediate safety upgrade.
Why This Matters for Healthcare Communication United Kingdom
In a healthcare system already stretched to capacity, slow communication is unacceptable.
Real-time communication:
- increases patient safety
- reduces clinical risk
- improves audit outcomes
- reduces stress for staff
- supports faster clinical decisions
- ensures the right people always get the message
Modernising internal communication is no longer optional — it's an urgent priority.
#6. Frontline Burnout Caused by Information Overload
Frontline healthcare staff are under more pressure than ever.
Long shifts, high patient loads, staffing shortages, and constant regulatory changes already push teams to the limit.
But one problem makes everything worse — information overload.
Ironically, healthcare staff often get too much information — just not the information they actually need. Alerts, emails, updates, reminders, notices, tasks, system messages… it never ends.
And this constant flood of unfiltered communication is one of the biggest contributors to burnout across teams.
The Problem: Too Many Systems, Too Many Alerts
Healthcare teams shouldn't need a map just to figure out where information is stored.
But in many hospitals, a single update might be hiding in:
- shared drives
- WhatsApp groups
- Microsoft Teams
- EHR notes
- printed memos
- staff noticeboards
- pagers
- personal notebooks
The average frontline worker toggles between 5 to 9 different communication systems every shift.
No one can keep up with that — especially not in a high-pressure clinical environment.
This leads to:
- missed updates
- constant interruptions
- decision fatigue
- stress and confusion
- lower performance
- inconsistent task follow-through
It becomes impossible to tell what's important and what's just noise.
How Cognitive Overload Leads to Mistakes
Information overload doesn't just stress staff — it affects patient care.
When frontline teams are drowning in communication, the brain starts filtering automatically.
The problem?
It's filtering based on survival, not priority.
Cognitive overload causes:
- slower reaction times
- reduced attention to detail
- missed warning signs
- increased errors
- emotional exhaustion
- difficulty prioritising
- irritability and poor communication
Healthcare workers aren't machines. When too many inputs hit at once, mental capacity collapses.
UK Burnout Data Linked to Communication Chaos
Burnout is now one of the largest workforce challenges in UK healthcare.
According to studies by the King's Fund, NHS Providers, and BMJ:
- 51% of UK healthcare staff say communication overload contributes to burnout
- Staff receive over 120+ notifications per shift (email + systems + alerts)
- 1 in 3 nurses say they miss important updates because there are too many channels
- Burnout increases clinical error risk by 2.3x
- 40% of staff say they're overwhelmed by the number of systems they must use daily
Burnout isn't caused by workload alone — it's caused by chaotic communication around the workload.
The Solution: Consolidation Into One Simple Platform
The cure for information overload isn't more tools — it's fewer tools.
Frontline teams need one single communication platform where:
- updates
- tasks
- alerts
- policies
- announcements
- handovers
- compliance messages
- documents
…all live in one place, instead of being scattered across the organisation.
AgilityPortal solves this by consolidating communication into a single, modern digital workplace that reduces noise and boosts clarity.
One Login for Everything
Instead of juggling 9 different systems, staff log into one secure hub for:
- messaging
- shift updates
- training
- tasks
- documents
- compliance alerts
- team announcements
- clinical resources
This cuts cognitive load instantly.
Personalised Updates Instead of Global Spam
Frontline staff don't need everything — they only need what's relevant to their role, their ward, and their patients.
AgilityPortal delivers:
- role-based updates
- ward-specific alerts
- personalised dashboards
- filtered communication
- reduced noise
This ensures the right people get the right message — and only that message.
Streamlined Daily Workflows
AgilityPortal supports staff through:
- to-do lists
- priority flags
- integrated clinical notes (if connected)
- simplified handovers
- reminders
- structured update feeds
This turns chaotic days into predictable workflows, reducing stress and improving care quality.
The Result: Less Overload, Less Burnout, More Clarity
When teams move to a single, consolidated communication platform, the impact is immediate:
- Fewer missed updates
- 25–40% fewer daily interruptions
- Higher staff satisfaction
- Clearer prioritisation
- Better decision-making
- Lower turnover rates
- Higher quality of patient care
Frontline teams can breathe again — mentally and emotionally.
Why This Matters for Healthcare Communication United Kingdom
Burnout isn't just a wellbeing issue — it's a patient safety issue.
When communication is overwhelming, mistakes rise.
When communication is clear, safe, and consolidated — mistakes fall.
Modernising communication is one of the fastest ways to:
- reduce staff burnout
- improve retention
- strengthen patient safety
- support compliance
- create calmer, more predictable shifts
This is where communication upgrades make a real, human difference.
#7. Lack of Staff Feedback Loops and Patient-Facing Insights
One of the biggest gaps in healthcare communication united_kingdom isn't just how information flows to staff — it's how information flows back from them.
Most UK healthcare organisations still rely on outdated or inconsistent methods to gather feedback:
- verbal comments
- suggestion boxes
- anonymous notes
- occasional annual surveys
- staff trying to raise issues via email
- informal conversations during shifts
None of these create a reliable feedback loop. And without structured insight, leaders have no clear picture of how teams feel, what problems they're facing, or where risks are emerging.
This is one of the most damaging healthcare communication challenges UK because without feedback, problems stay hidden until they explode.
The Problem: Leadership Doesn't Have Real-Time Insight
When feedback is unstructured and inconsistent, leaders struggle to understand:
- staff morale
- operational friction
- burnout indicators
- unsafe workloads
- communication failures
- training gaps
- workflow bottlenecks
- patient experience issues
It becomes a guessing game.
This means issues that could have been fixed early often become:
- disciplinary cases
- patient complaints
- safety incidents
- compliance breaches
- preventable burnout
- staff turnover
Healthcare teams want to be heard — but the systems to listen simply don't exist.
How Missing Feedback Creates Blind Spots
Without effective staff insight, organisations face several risks:
- Patient-care errors go unreported
- Rising workloads aren't flagged early enough
- Process failures grow unchecked
- Communication breakdowns aren't identified
- Toxic cultures go unnoticed
- Low morale becomes normal
- Staff disengagement impacts the quality of care
Poor feedback loops also create distrust.
When staff don't feel heard, they stop speaking up.
This is one of the biggest contributors to the broader issue of healthcare workforce engagement UK.
UK Data on the Impact of Poor Feedback Structures
The numbers are alarming:
- 44% of healthcare workers in the United Kingdom say they don't feel heard by leadership (NHS Staff Survey, 2024).
- Organisations without effective feedback systems experience 19% higher patient safety incidents.
- Units with regular pulse surveys report 23% fewer escalations.
- 1 in 3 NHS staff say they avoid reporting issues because the process is unclear or too slow.
Without transparent feedback mechanisms, both patient and staff safety decline.
The Solution: Built-In Feedback and Analytics
To fix the feedback gap, healthcare organisations need a structured, digital system that captures staff insights continuously — not once a year.
AgilityPortal provides a modern feedback ecosystem designed for clinical communication, patient safety communication UK, and healthcare workforce engagement UK.
Anonymous Pulse Surveys
Short, regular micro-surveys help capture:
- morale
- workload stress
- communication issues
- training needs
- team culture
- safety concerns
Because they're anonymous, frontline staff feel safe telling the truth.
Sentiment Tracking Over Time
AgilityPortal includes sentiment analytics that highlight:
- rising frustration
- communication breakdowns
- burnout indicators
- departmental stress trends
- compliance-related concerns
This allows leaders to act before problems escalate.
Issue Reporting and Trend Insights
Staff can quickly report:
- patient incidents
- communication failures
- missing equipment
- unsafe workloads
- policy confusion
- environmental risks
Everything is logged, tracked, and visible to managers — creating accountability and transparency.
This replaces outdated approaches like paper incident forms or informal emails, making your organisation more aligned with digital communication solutions for healthcare.
Why Strong Feedback Loops Matter for Healthcare Communication United Kingdom
When feedback is captured consistently and analysed properly:
- patient care improves
- risks are spotted early
- staff feel valued and heard
- leadership makes better decisions
- communication becomes two-way, not top-down
- compliance improves because issues are visible
- turnover decreases
- culture strengthens
Feedback turns healthcare teams from reactive → proactive.
It is one of the most cost-effective ways to improve patient safety, staff wellbeing, and organisational performance.
The Bottom Line: Insight Creates a Safer, Stronger Workforce
Effective feedback isn't just about morale — it's about:
- reducing clinical risk
- improving care consistency
- catching communication failures early
- strengthening NHS workforce retention
- improving the patient experience
When staff have a voice, the entire organisation becomes stronger.
How to Fix All 7 Problems With AgilityPortal
After breaking down the top communication challenges in UK healthcare — siloed teams, outdated tools, missing handover standards, compliance confusion, slow escalation, information overload, and weak feedback loops — one truth becomes clear:
These problems cannot be solved by adding more tools.
They can only be solved by replacing fragmentation with one unified communication platform.
Healthcare teams don't need 10 systems.
They need one digital workspace that brings everything together.
This is where AgilityPortal transforms healthcare communication united_kingdom with a modern, unified solution built around speed, clarity, and safety.
Why Fragmented Tools Will Always Fail
Fragmented systems fail because:
- staff don't know which tool to use
- information gets duplicated
- updates get lost
- leaders can't track what staff have seen
- systems don't talk to each other
- frontline staff don't have time to check multiple platforms
- critical alerts reach the wrong people
In UK healthcare settings, this fragmentation leads to:
- patient delays
- safety incidents
- compliance failures
- resource waste
- burnout
- outdated practice
Fragmented communication = inconsistent care.
Why Centralisation Is Critical in Modern Healthcare
When communication is centralised:
- every team sees the same information
- shift handovers become consistent
- compliance documents stay current
- frontline staff get only the updates relevant to them
- leaders get real-time visibility
- emergency alerts reach the right people instantly
- burnout decreases due to fewer systems
- learning, policies, documents, and tasks all connect
A centralised digital workplace becomes the backbone of the entire care environment.
This is the future of digital communication solutions for healthcare across the United Kingdom.
How AgilityPortal Solves Communication Gaps End-to-End
AgilityPortal is designed to eliminate the exact barriers blocking communication inside NHS Trusts, private clinics, care homes, and community healthcare providers.
Here's how:
AI-Powered Search for Lightning-Fast Information Retrieval
Staff no longer waste 30–60 minutes a shift searching for:
- policies
- treatment guidelines
- forms
- SOPs
- escalation pathways
- announcements
AI search instantly finds the correct version — removing confusion and saving valuable time during patient care.
Version Control and Compliance Logging
Every document is:
- version-controlled
- audit-ready
- tracked with timestamps
- monitored for expiry
- linked to responsible owners
Compliance teams finally get full visibility — and no more outdated files.
Mobile App for Frontline Teams
Frontline teams get:
- real-time alerts
- shift updates
- clinical messages
- urgent notifications
- team channels
- safe, role-based communication
This removes reliance on pagers, WhatsApp, or email for critical information.
Spaces for Clinical, Admin, and Support Teams
Each department gets its own tailored digital space:
- wards
- theatres
- admin teams
- labs
- imaging
- community care
- pharmacy
- estates & facilities
This reinforces structure, clarity, and shared understanding.
Real-World Results From UK Healthcare Teams
Healthcare organisations using AgilityPortal typically see:
- up to 40% faster internal communication
- fewer handover errors
- better compliance outcomes during CQC inspections
- reduced clinical incidents linked to miscommunication
- improved patient flow between departments
- higher staff satisfaction and retention
- less burnout due to fewer systems and clearer communication
Modern, unified communication isn't "nice to have."
It's one of the most effective ways to improve patient safety and operational performance.
Conclusion
Healthcare in the United Kingdom is under immense pressure — rising patient numbers, workforce shortages, increasing regulatory demands, and tighter accountability. But underneath all of these challenges sits one core issue:
Across NHS Trusts, private hospitals, speciality clinics, and care homes, communication determines:
- how safe patients are
- how effective teams are
- how fast decisions are made
- how well compliance is maintained
- how confident staff feel
- how much burnout rises or falls
The seven challenges we explored — silos, outdated tools, handover inconsistencies, poor policy visibility, slow escalation, information overload, and weak feedback loops — all point to one undeniable truth:
Healthcare communication united kingdom needs to be modernised.
The organisations thriving today are the ones that have moved beyond outdated systems and invested in one centralised digital workplace that connects every department, every shift, every role.
AgilityPortal gives healthcare organisations exactly that:
- faster communication
- safer handovers
- real-time alerts
- better compliance
- clearer information flow
- empowered staff
- unified teamwork
- less stress
- better patient outcomes
When communication improves, everything improves.
- Better care.
- Better safety.
- Better staff wellbeing.
- Better operational performance.
- Better trust from regulators.
The future of healthcare doesn't just depend on technology — it depends on communication done right.
Categories
Blog
(2726)
Business Management
(333)
Employee Engagement
(213)
Digital Transformation
(185)
Growth
(124)
Intranets
(121)
Remote Work
(61)
Sales
(48)
Collaboration
(43)
Culture
(29)
Project management
(29)
Customer Experience
(26)
Knowledge Management
(21)
Leadership
(20)
Comparisons
(8)
News
(1)
Ready to learn more? 👍
One platform to optimize, manage and track all of your teams. Your new digital workplace is a click away. 🚀
Free for 14 days, no credit card required.